
When was the last time you visited a doctor and the first thing asked of you was to show your tongue? Western medical practice of tongue diagnosis as part of a routine clinical examination seems, like many Western clinical practices, to have become a relic of the not-too-distant past.
Instead, it survives as a standard of practice routinely employed as part of Traditional Chinese Medicine (TCM), Ayurvedic medicine, and used by some naturopaths and herbalists.
While there are similarities between old Western medical and traditional Eastern tongue diagnosis, some of the differences can serve to amplify what can be learned with each of these methods.
To begin, one of the ground rules for both approaches is that tongue diagnosis is only one aspect of differential diagnosis which evaluates and compares several different diagnosis parameters. This means that there are exceptions to practically every diagnostic finding which require further verification.
Secondly, even though we will confine our presentation in this short presentation to the tongue, it is generally recognized that its traditional partner, pulse analysis, evaluates the condition of the body-mind from the perspective of the cardiovascular and nervous system, while the tongue, offers information on the health of the body from the perspective of the digestive system.

Since traditional medicine generally considers that disease originates or is intimately involved with the GI tract, tongue diagnosis is an excellent place to analyze and form treatment strategies for those whose practice is largely based on dietary and herbal treatments.
As a point of reference let’s begin with a photograph of how a normal tongue should appear:
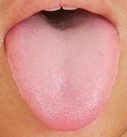
The aspects of the tongue that are considered include its shape, body, and coat. A normal tongue body is a healthy pink color, with a slight coat, and a shape that neither too large, nor too small and horseshoe shape. Deviations from these parameters can indicate genetic or acquired imbalances.
Now, with no attempt to be exhaustive of all the different tongue appearances, let’s consider some of the more common and obvious imbalances based on Western medical clinical findings and TCM.
Some Western and TCM tongue diagnostic indications
The scarlet red tongue with little or no coat


The tongues above share the characteristics of a very red tongue body with little or no coat. TCM would describe this as an indication of empty or deficient heat evidenced by the heightened red body, yin deficiency because of the lack of coat, and in the second tongue deeper ruts and fissures. In TCM Yin deficiency indicates a lack of moisture, dryness and sympathetic (Kidney* Yang) excess and parasympathetic (Kidney* Yin) deficiency. The fissure down the center specifically indicates digestive (Spleen*) deficiency.
* Keep in mind that the TCM explanation of physiology has not progressed for approximately 300 years, so Western medical doctors attempting to understand TCM theory have to adjust for terms they use in common, but which have very different meanings. For example, the TCM Kidneys refer to both the urinary organs but also the adrenals and endocrine system. The TCM Spleen hardly describes simple physiological spleen functions as a blood filter but refers to the complex effect of the functions of the pancreas and the deeper levels of digestion and assimilation.
The treatment strategy for this type of tongue is to nourish Yin and clear deficient or empty heat. Yin deficiency, which is a progression from Blood deficiency, requires nutritional treatment with warm, moist, fatty proteinaceous foods such as pork, salmon, beef; vegetables such as okra, cooked vegetables with olive oil, mushrooms or ghee; fruit such as avocados, plantains or bananas; and Yin nourishing and anti-inflammatory herbs with cooling, demulcent properties. For more severe cases of Yin deficiency with heat, the TCM formula known as Zhi Bai Di Huang, also known as Anemarrhena and Phellodendron Combination can be used. For Yin deficiency with little or no heat, Rehmannia Six is recommended.
Anemarrhena and Phellodendron combination (Zhi Bai Di huang wan)
| Anemarrhena rhizome | (Anemarrhena asphodeloides) | (Zhi Mu) |
| Phellodendron bark | (Phellodendron chinense) | (Huang Bo) |
| Rehmannia root cured | (Rehmannia glutinosa) | (Shu Di Huang) |
| Asiatic dogwood fruit | (Cornus officinalis) | (Shan Zhu Yu) |
| Tree peony bark | (Paeonia suffruticosa) | (Mu Dan Pi) |
| Chinese yam rhizome | (Dioscorea opposita) | (Shan Yao) |
| Poria sclerotium | (Poria cocos) | (Fu Ling) |
| Asian water plantain rhizome | (Alisma orientale) | (Ze Xie) |
https://bit.ly/39ggNbM or https://bit.ly/3btQ5iO
Rehmannia Six Combination (Liu wei di huang)
| Rehmannia root cured | (Rehmannia glutinosa) | (Shu Di Huang) |
| Asiatic dogwood fruit | (Cornus officinalis) | (Shan Zhu Yu) |
| Tree peony bark | (Paeonia suffruticosa) | (Mu Dan Pi) |
| Chinese yam rhizome | (Dioscorea opposita) | (Shan Yao) |
| Poria sclerotium | (Poria cocos) | (Fu Ling) |
| Asian water plantain rhizome | (Alisma orientale) | (Ze Xie) |
https://bit.ly/39ozie2 or https://bit.ly/38wYWxY
In most cases since yin deficiency involves the body’s essence, one may need to take these herbs for at least 3 months but often much long to achieve significant results on the tongue.
On the other hand, the Western medical assessment for a scarlet red tongue with little or no coat, would be Vitamin B/B12 deficiency.
There are two major reasons for B12 and general B vitamin deficiency. One is lack of consumption of B-rich foods, but the second reason, which is undoubtedly more often an issue especially if people are consuming animal foods as part of their diet, is problems with assimilation.
For example, many elderly people experience signs of B12 deficiency such as chronic low energy due to a lack of intrinsic factor. Intrinsic factor is a glycoprotein found in the lining of the stomach and small intestines which is necessary for the absorption and utilization of B vitamins, especially B12, folic acid and riboflavin. Intrinsic factor and other digestive secretions such as bile produced by the liver, are components of digestion that tend to fluctuate throughout life, tending to be more consistently lacking with age.
Besides a proteinaceous diet with cooked green vegetables and probiotic foods, certain herbs play a role in promoting digestion including Western digestive bitters such as angostura bitters sold in most liquor stores, or Ayurvedic Draksha which is ayurvedic low-alcohol wine made from fermented grapes and herbs. A great digestive bitters combination would be my own Planetary Digestive Grape Bitters together with Planetary Triphala tablets. You can find these and more in the Planetary Herbals store.
